JCU researchers drive meaningful change
A James Cook University research team has harnessed data to create an open-access, interactive map that empowers northern Queensland communities to have a say in health service planning.
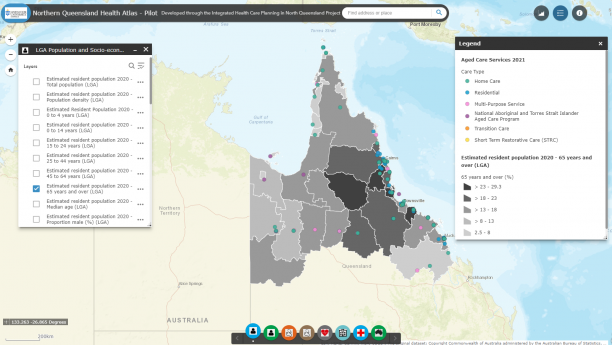
The map, called the Northern Queensland Health Atlas, is an open-access digital tool that gives users the ability to filter and overlay data on the burden of disease or ill health, socio-demographic information, the availability of general practice and other specialist services, as well as indicators of health system performance in specific geographic areas.
The atlas is a key component of the three-year Integrating Health Care Planning for Health and Prosperity in North Queensland project, developed to pilot the principles of place-based planning. The project is funded by the Cooperative Research Centre for Developing Northern Australia (CRCNA), part of the Australian Government’s Cooperative Research Centre Program (CRCP), with a financial contribution from the Tropical Australian Academic Health Centre (TAAHC).
Community members in the north west Queensland town of Hughenden will soon be the first to trial place-based health service planning using the health atlas data. It is anticipated the project will extend to another three communities across northern and central Queensland.
CRCNA CEO Anne Stünzner said place-based planning was crucial to ensure the best use of resources for the best possible return at all levels of health planning. “The CRCNA is excited the health atlas is a first step toward a much broader application of this principle,” Ms Stünzner said.
"This project is a great example of industry-led research driving meaningful outcomes for communities, giving people on the ground something tangible to coalesce around and advocate for."
Planning unique to communities
Co-investigator, JCU Associate Professor Stephanie Topp, said the atlas addressed one of the main barriers to place-based health planning: data accessibility. “The information that would shape decisions about how a health service could or should run is located in so many different places, not just within Queensland but Australia,” A/Prof Topp said.
“The idea of place-based planning is to bring the data and the decision-making processes around health service formation and coordination closer to the communities themselves. The health atlas increases the accessibility and agility with which health needs can be compared to service access and availability. Joined-up information like this is the basis of good planning and efficient use of resources. The atlas, as a proof of concept, is an important flag for the need for something like this at a much larger scale.”
Advocacy and change at local level
In the second phase of the three-year project, community members will use the atlas data and local knowledge to identify opportunities to improve efficiencies in health service delivery. Community members will be involved in co-design discussions to identify local issues and contribute to developing strategies that can be implemented through the project.
Local project officers will help facilitate a series of workshopped discussions with local stakeholders, including community members and health providers, on the health needs indicated in the atlas, guided by a collaborative reference group who will identify feasible actions to address gaps at the local level. Whilst the project concludes in April 2024, changes aim to be sustainable beyond the project.
The project is a partnership with TAAHC, including the five northern hospitals and health services, the NQ Primary Health Network and Queensland Aboriginal and Islander Health Council. Partners from the Northern Territory and Kimberley are also involved.
A/Prof Topp said a goal of the project was to create a process that allowed local stakeholders to participate in and regain control of some of the healthcare decision making in their communities, generating the momentum to address structural issues through advocacy.
“There's a dual benefit of taking control of those pieces that are able to be managed at a local level and empowering people to have a louder and more assertive voice when it comes to advocating for change at the central level,” she said.

Democratising data
Along with A/Prof Topp, the JCU research team comprises lead investigator Professor Sarah Larkins with co-investigators Professor Maxine Whittaker, Dr Alex Edelman, Dr Nishila Moodley, project manager Dr Deb Smith, data manager Dr Karen Johnston, and health economist Mr Chris Rouen.
Dr Smith and Dr Johnston sourced the atlas statistics from many different databases, including the Australian Institute of Health and Welfare, Federal Department of Health, the Australian Bureau of Statistics and Queensland Health.
A/Prof Topp said the challenges the two highly skilled JCU researchers faced in locating, curating, and collating the health atlas data for northern Queensland emphasised the disparate nature of Australia’s data ecosystem.
"We need to democratise access to this publicly funded, publicly collected data."
“Data, without malign intent, is inaccessible nonetheless to the vast majority of Australians. It takes significant research, expertise, diligence, time and money to curate it in a way that makes it usable by the average service planner or programmer, let alone a service provider. Making that data more accessible to everyone in the health system, including those who need to use it, can only serve to better inform and promote the sorts of decisions that will produce better health outcomes.
“We are pulling together a paper which reflects on our experience and the effort that had to be put into locating the data, de-duplicating it, extracting the information that was applicable to the different geographic boundaries to which it's applied, and then bringing it together in a form that was easily usable by someone who wasn't necessarily a computing genius.”
She said the Northern Queensland Health Atlas was intuitive and operable by users at all levels. “We should have a tool like this for the whole country,” she said. “It is astounding that we continue to plan services in the absence of joined-up information about health needs, service access and service performance. Every community should be able to look at their own profile.”
Dr Stünzner said the CRCNA’s 2020 health situational analysis on health service delivery, led by the same JCU team, clearly identified the need for improved access to accurate and timely data to better inform decision making across all levels of health funding and planning. “It’s great to see this team building on their earlier work and addressing this gap to the benefit of the broader Northern Australian community,” she said.
A/Prof Topp said the atlas had generated excitement among project partners and industry stakeholders. “We knew intuitively that there wasn't a tool like this easily available, but I think we had underestimated the enthusiasm for getting over the hump of making a start,” she said. “The fact that people can now see what this atlas makes available has really produced a lot of enthusiasm for seeing how we can further build on it.”
Explore the Northern Queensland Health Atlas
Watch the Northern Queensland Health Atlas Launch Webinar | Meet members of the research team from James Cook University and Cooperative Research Centre for Developing Northern Australia, who will discuss the project, guide you through the atlas and its benefits, and highlight data challenges.