A practical experience
Originally from Melbourne, Sixth-year JCU Medicine student Isabella Stewart recently set out on her final-year rural placement on Thursday Island. Over the next 10 weeks she learned the vast scope of medicine that rural doctors face, coming to a humble discovery.
During my rural term I was rostered to the emergency department, general ward, and general practice. I also had the chance to work in surgery for endoscopies, attend clinics and assist in surgery with the gynaecology outreach team from Cairns.
In terms of practical work, I was excited to undertake the role of an intern under supervision. In the emergency department, this involved seeing patients before the doctors, taking a history, conducting an examination, ordering investigations and developing a preliminary management plan. We presented our findings to the doctor and they would confirm or adapt the management plan. I also helped the doctors put dislocated bones back in place and apply casts, which was a fantastic opportunity to consolidate and build on the knowledge I’ve gained over the years of studying medicine at JCU.
On the medical ward we would write ward notes, follow up on patient results, do cannulas, take bloods, and assist with referrals where required. This was particularly good practice for being an intern as one of the more daunting things as a junior doctor is calling senior doctors for referrals, usually to ask for treatment advice or request a transfer to their care.
In the general practice clinic, I was given my own consult room and was able to independently see walk-in patients before discussing their care with the supervising doctor.
I was also extremely fortunate to accompany the doctors on their outreach clinics to some of the outer islands. These day trips involved flying by helicopter to the island, seeing patients in clinic during the day, then flying home in the afternoon. It was a huge privilege to be welcomed on to these remote islands and learn about these communities.

In the midst of an outbreak
Being on placement on Thursday Island during a global pandemic meant that I saw many upper respiratory infections in the emergency department, more than one would normally expect. Anybody with a runny nose, cough, or any symptoms of a fever for that matter, would be sent directly to the fever clinic in the emergency department. This often meant the patient was reviewed by a doctor for a relatively minor cold. Despite making the emergency department busier than usual, it’s fantastic that the community was being diligent and getting tested. This was particularly reassuring in the last few weeks of my placement, as PNG was in the midst of a COVID outbreak.
They started vaccinating the islands closest to PNG during my final week on the island. When the opportunity arose, I was able to discuss the vaccine with my patients and reassure them that the vaccine was safe and effective.
Coming away with a new perspective
I learnt a lot about retrieval and remote medicine and the nuanced implications for medical care. My biggest take away from my rural placement in a rural community is that access to advanced interventions such as specialist surgery or the intensive care unit is many hours away. This affects how we treat patients; for example, a patient with mild symptoms but many complicated medical conditions might be transferred to Cairns, whereas a younger patient with the same symptoms and fewer background conditions might be monitored on Thursday Island.
I have also witnessed how broad the scope of practice is for these doctors, and how hands-on rural medicine can be, especially with high acuity cases. These doctors can be thrombolysing someone with a heart attack in the morning, administering a general anaesthetic in the afternoon, and then flying in a helicopter to pick up a patient with sepsis in the evening. And this is considered a standard day at work!
One of the most acute cases I was involved in was an unconscious patient with ongoing seizures and a high fever who had viral encephalitis. I had the opportunity to assist in the intubation prior to the Rural Flying Doctors Service arriving to transfer the patient to a larger hospital.
It’s been humbling to learn that rural medicine is so much more than ‘just general practice’. With the vast scope of medicine that rural doctors face, I have come to appreciate the immense skill set and knowledge that our rural and remote doctors have.
An island lifestyle
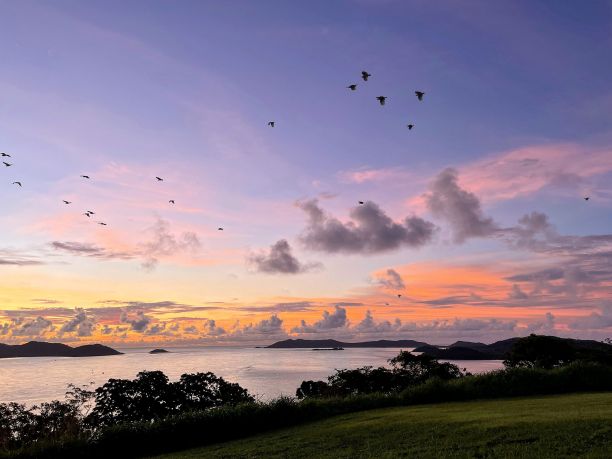
We visited a number of waterfalls on the adjacent Prince of Wales Island, went fishing with some of the locals, and watched many, many sunsets. I can’t understate how fulfilling this placement was. The additional independence we had on placement allowed me to consolidate my communication, practical and examination skills in preparation for my intern year next year. My favourite thing about the community is that everyone I passed on the street offered a smile and said “Morning/Afternoon/Evening”. It was an absolute pleasure learning about the Torres Strait culture and community I had the honour to be a part of.
Isabella has completed the last two clinical years in Cairns, and will be returning to Cairns Hospital for the remainder of this year to complete her studies.