The LEAP Project
LEAP Storyboard Part 1
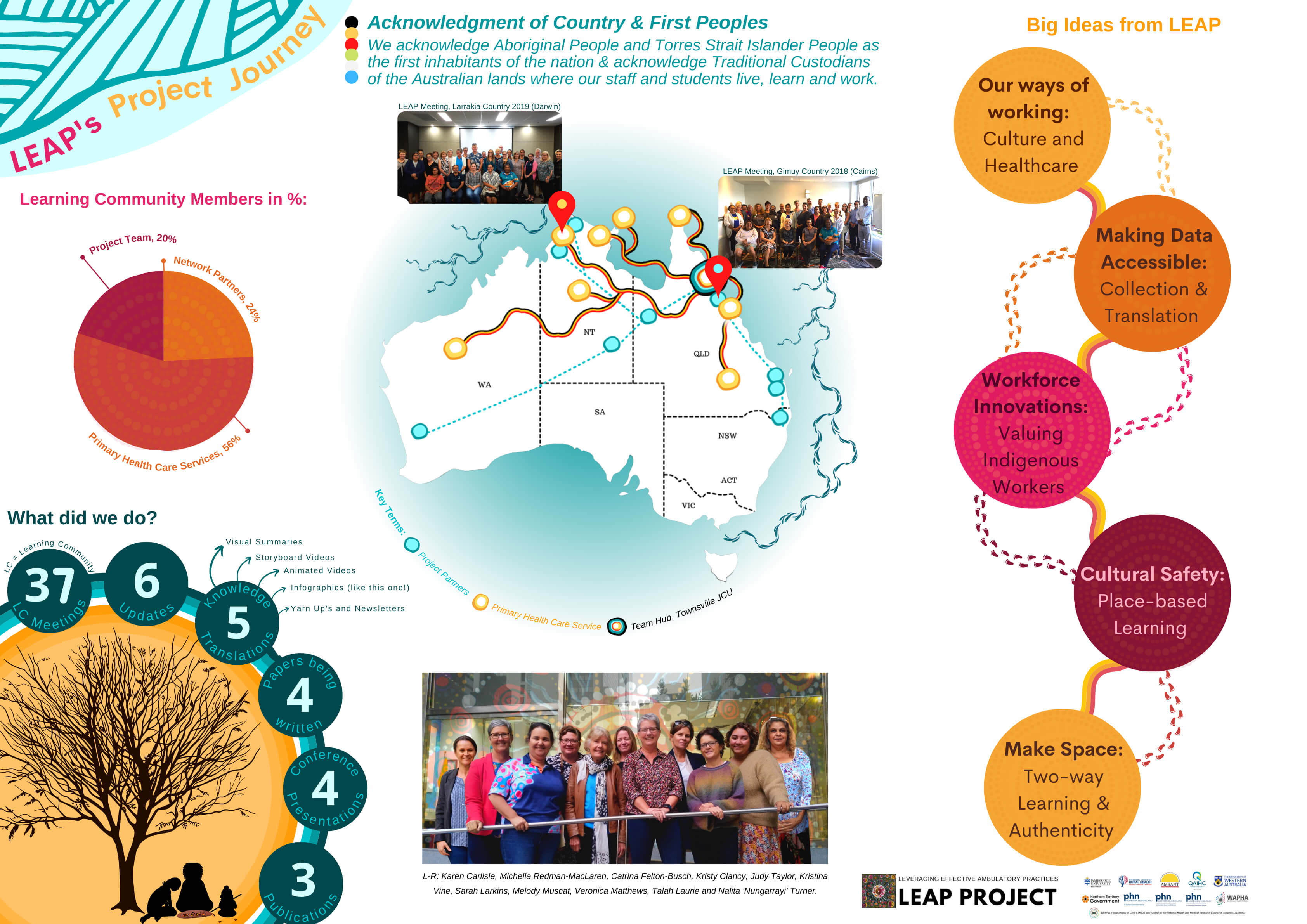
Leveraging Effective Ambulatory Practices
LEAP Storyboard Part 2
The LEAP (Leveraging Effective Ambulatory Practices) project aims to work with Aboriginal and Torres Strait Islander primary health care services to identify and implement a strengths-based framework that will support quality improvement – we seek to understand what is needed for all services to succeed.
Why is this project needed?
Primary health care services are made up of many systems, and successful change depends upon a good “match” between the realities for the service and actions for improvement. Despite increased policy attention and funding, not all primary health care services for Aboriginal and Torres Strait Islander Australians have shown improvements in quality of care despite continuous quality improvement action. We need to understand the challenges to reaching quality of care goals, what is needed to overcome these challenges and how acceptable and effective a toolkit of interventions might be to improve quality of care.
How we will do this project?
Working in partnership in Aboriginal and Torres Strait Islander health is fundamental, and this project builds on current work and existing partnerships to improve the quality of health services. Working with eight Aboriginal and Torres Strait Islander primary health care services and existing quality improvement networks, we will support services to achieve their quality improvement goals.
Specifically, we will co-create a Learning Community that centralises services, we will conduct case studies to identify implementation challenges and their interactions, and then collaborate to develop a toolkit to address the identified challenges. Services will then be supported to implement useful elements of the toolkit to address their most important quality of care needs. Throughout joint project assessments will be conducted to understand the effectiveness, impact and acceptability of the interventions.
This project will help us understand how to best support services to successfully implement changes that will overcome challenges and improve the quality of Aboriginal and Torres Strait Islander health services for better health outcomes.
Project Updates
Presentations
Respect is Central
A Critical Review of Implementation Frameworks for CQI in Aboriginal and Torres Strait Islander PHC Services
Talking Grounds
Building togetherness from a distance in Indigenous PHC research. Presented by Talah Laurie and Kris Vine @ the 8th Rural and Remote Health Scientific Symposium, October 2021
Publications and research translations
Respect nalita short
Reflections on centralising respect in PHC services with Nalita Nungarrayi Turner
Turner, N. N., J. Taylor, S. Larkins, K. Carlisle, S. Thompson, M. Carter, M. Redman-MacLaren and R. Bailie (2019). "Conceptualizing the Association Between Community Participation and CQI in Aboriginal and Torres Strait Islander PHC Services." Qualitative Health Research: 1049732319843107.
Redman-MacLaren, M., Turner , N. N., Taylor, J., Laycock, A., Vine, K., Thompson , Q., . . . Matthews , V. (2021). Respect Is Central: A Critical Review of Implementation Frameworks for Continuous Quality Improvement in Aboriginal and Torres Strait Islander Primary Health Care Services. Frontiers in Public Health, 9(926). doi:10.3389/fpubh.2021.630611
Carlisle K, Matthews Quandamooka V, Redman-MacLaren M, et al. A qualitative exploration of priorities for quality improvement amongst Aboriginal and Torres Strait Islander primary health care services. BMC Health Serv Res. 2021;21(1):431. Published 2021 May 6. doi:10.1186/s12913-021-06383-7
"Respect is Central": The Honey Ant Story
NHMRC Partnership Grant Idea from LEAP (CRE-STRIDE Stream 2)
LEAP Learning Community Resources
Below is a list of resources that may help support your improvement work in your health centre, or support someone doing that work. You may access a resource by clicking on the title of the resource or the website address.
If you cannot access a resource in the list below, please email your friendly LEAP Project team on leap@jcu.edu.au
Gardner, K., Sibthorpe, B., Chan, M., Sargent, G., Dowden, M., & McAullay, D. (2018). Implementation of continuous quality improvement in Aboriginal and Torres Strait Islander primary health care in Australia: a scoping systematic review. BMC Health Services Research, 18(1), 541. doi:10.1186/s12913-018-3308-2
Larkins, S. et al (2017). The implementation gap: what is needed to ensure the effectiveness of quality improvement interventions in Indigenous primary health care? PHC Research conference, Brisbane, August 2017 (Presentation; full text available).
NACCO (2019). National Framework for Continuous Quality Improvement in Primary Health Care for Aboriginal and Torres Strait Islander people, 2018-2023. https://www.naccho.org.au/programmes/cqi/
Trask, L. (n.d.). Continuous Quality Improvement: Linking local implementation to state support and national policy. QAIHC (Presentation, includes links to videos; full text available).
Vaughn, V. M., Saint, S., Krein, S. L., Forman, J. H., Meddings, J., Ameling, J., . . . Chopra, V. (2019). Characteristics of healthcare organisations struggling to improve quality: results from a systematic review of qualitative studies. BMJ Quality & Safety, 28(1), 74. doi:10.1136/bmjqs-2017-007573
Atkins, L., Francis, J., Islam, R., O’Connor, D., Patey, A., Ivers, N., . . . Michie, S. (2017). A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implementation Science, 12(1), 77. doi:10.1186/s13012-017-0605-9
Beaton, A., Manuel, C., Tapsell, J., Foote, J., Oetzel, J. G., & Hudson, M. (2019). He Pikinga Waiora: supporting Māori health organisations to respond to pre-diabetes. International Journal for Equity in Health, 18(1), 3. doi:10.1186/s12939-018-0904-z
Damschroder, L. J., Aron, D. C., Keith, R. E., Kirsh, S. R., Alexander, J. A., & Lowery, J. C. (2009). Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science, 4(1), 50. doi:10.1186/1748-5908-4-50
French, S. D., Green, S. E., O’Connor, D. A., McKenzie, J. E., Francis, J. J., Michie, S., . . . Grimshaw, J. M. (2012). Developing theory-informed behaviour change interventions to implement evidence into practice: a systematic approach using the Theoretical Domains Framework. Implementation Science, 7(1), 38. doi:10.1186/1748-5908-7-38
Graham I, Tetroe JM In: Rycroft Malone J, Bucknall T, editors. Models and frameworks for implementing evidence-based practice: linking evidence to action. Chichester, England: Wiley-Blackwell; 2010. p. 207–22.
Kitson, A. L., Rycroft-Malone, J., Harvey, G., McCormack, B., Seers, K., & Titchen, A. (2008). Evaluating the successful implementation of evidence into practice using the PARiHS framework: theoretical and practical challenges. Implementation Science, 3(1), 1. doi:10.1186/1748-5908-3-1
Meyers, D. C., Durlak, J. A., & Wandersman, A. (2012). The Quality Implementation Framework: A Synthesis of Critical Steps in the Implementation Process. American Journal of Community Psychology, 50(3-4), 462-480. doi:10.1007/s10464-012-9522-x
Newham, J., Schierhout, G., Bailie, R., & Ward, P. R. (2016). ‘There’s only one enabler; come up, help us’: staff perspectives of barriers and enablers to continuous quality improvement in Aboriginal primary health-care settings in South Australia. Australian Journal of Primary Health, 22(3), 244-254. doi:https://doi.org/10.1071/PY14098
Smith, G., Kirkham, R., Gunabarra, C., Bokmakarray, V., & Burgess, C. P. (2019). 'We can work together, talk together': An Aboriginal Health Care Home. Australian Health Review, 43(5), 486-491. doi:10.1071/AH18107
Deroy, S., & Schütze, H. (2019). Factors supporting retention of aboriginal health and wellbeing staff in Aboriginal health services: a comprehensive review of the literature. International Journal for Equity in Health, 18(1), 70. doi:10.1186/s12939-019-0968-4
CRANAplus (2013). A clinical governance guide for remote and isolated health services in Australia (Full text available)
Laycock, A., Bailie, J., Matthews, V., & Bailie, R. (2019). Using developmental evaluation to support knowledge translation: reflections from a large-scale quality improvement project in Indigenous primary healthcare. Health Research Policy and Systems, 17(1), 70. doi:10.1186/s12961-019-0474-6
- NT Health (2018) Health Advisory Committees Fact Sheet and Terms of Reference. https://digitallibrary.health.nt.gov.au/prodjspui/handle/10137/1300
- Molyneux, et al. (2012). Community accountability at peripheral health facilities: a review of the empirical literature and development of a conceptual framework (Open Access). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3465752/
- Taylor, Judy et al (2008) Working with Communities in Health and Human Services. Oxford University Press, South Melbourne, VIC, Australia.
- Apunipima Cape York Health Council (website). Health Action Teams http://www.apunipima.org.au/index.php/aurukun/62-about/governance
- Larkins S, Carlisle K, Turner N, et al. (2019) ‘At the grass roots level it’s about sitting down and talking’: exploring quality improvement through case studies with high improving Aboriginal and Torres Strait Islander primary healthcare services. (Open Access) BMJ Open https://bmjopen.bmj.com/content/9/5/e027568
- Turner, N. N., Taylor, J., et al (2019). Conceptualizing the Association Between Community Participation and CQI in Aboriginal and Torres Strait Islander PHC Services (Open Access). Qualitative Health Research. https://journals.sagepub.com/doi/10.1177/1049732319843107
AMSANT CQI PAGE: http://www.amsant.org.au/cqi/
Artwork by Noela Jimarin